

















|
 Janurary/Feburary, 1999 Volume XIII Number 4
Janurary/Feburary, 1999 Volume XIII Number 4
The Oral Contraceptive Pill: Can a Christian afford to take it?
by Chris Kahlenborn, M.D.
The oral contraceptive pill is currently being used by over 10 million women in the US 1, many of whom are reportedly Christian. A number of physicians and researchers have noted that the oral contraceptive pill (OCP) is actually an abortifacient (ie, an agent that causes an early abortion). They claim women who take it have early abortions, with some estimating that a woman experiences about one early abortion for every year she is taking it 2. Others have stated that they do not believe the OCP is an abortifacient as noted in the recent publication (1998), written by several physicians called: Hormonal Contraceptives: Are they Abortifacients? 23
Who is correct? This question is extremely important. It should be remembered that each of us was originally a tiny unborn child who consisted of only a few cells. Even our Lord Jesus appeared to have allowed Himself to pass through this tiny but critical stage. Obviously, Jesus was still Jesus at every point of His earthly existence and the same applies to us. The "worth" of a "tiny human being" must be judged to be the equivalent of that of a "big human being" and so we must be careful to protect and offer the same respect to the tiniest of our brothers and sisters.
The ethical question of whether contraception is morally permissible has varied among the Catholic Church and Protestant churches. Both agreed on the "sin of contraception" before 1930 3, while both differ in general on the issue today. This paper will focus on the medical and technical aspects concerning the noted questions regarding the pill's abortifacient qualities and refrain from commenting on the subject of its morality.
In order to answer the question of whether the OCP causes early abortions a number of basic questions need to be answered such as:
1) What is an oral contraceptive pill (OCP) and how does it work?
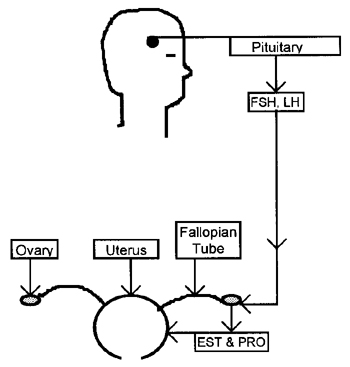
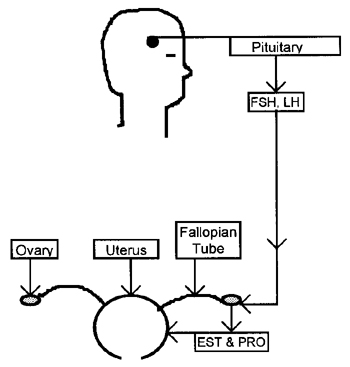
Normally, as we can see in diagram A, the pituitary gland produces two hormones called FSH (Follicle Stimulating Hormone) and LH (Luteinizing Hormone). These hormones serve to stimulate the ovary to produce an egg each month (ie, to ovulate). The ovary is also the site of production of the woman's two central female hormones, estradiol (EST), a type of estrogen, and progesterone (PRO), a type of progestin. Oral contraceptive pills (OCPs) are a combination of synthetic estrogen and progestin. Oral contraceptives "fool" the pituitary gland so that it produces less follicle stimulating hormone and luteinizing hormone. These two hormones are needed for ovulation to occur, therefore, OCPs suppress, but do not eliminate ovulation.
Oral contraceptives have two other main effects:
1) they thin the inner lining of the uterus (called the endometrium), depleting it in glycogen (ie, a type of sugar) and decrease its thickness. A thinner endometrium has a decreased blood supply.
2) they may serve to thicken the cervical mucus, making it more difficult for the sperm to travel up through the cervix. The evidence for this is weak 3A, 3B and not strongly supported by the rabbit model 3C.
Of course, OCPs could not cause abortions if they always stopped ovulation so this needs to be the first issue that is raised. A clear proof of the occurrence of ovulation is provided by noting what the drug companies which manufacture OCPs state. If one opens up the PDR (Physician's Desk Reference, c1998) one will find a table describing the "efficacy rate" of the OCP. In every table listed under each OCP one notes a "typical failure rate" of 3%. The PDR defines this as the rate of annual pregnancy occurrence noted in "typical couples who initiate use of a method (not necessarily for the first time) and who use it consistently and correctly during the first year if they do not stop for any other reason." This means that even couples who used the pill consistently over the course of a year had a pregnancy rate of 3%, proving that both ovulation and conception occur in couples who use the pill. A recent paper by Potter 3D gives an excellent overview of the matter. She notes that the most recent data point to a rate of pregnancy for "typical use" as being 7%, which is probably the more accurate statistic given the immediacy of her research data and the fact that today's OCPs are lower dose, theoretically permitting a higher rate of breakthrough ovulation.
2) Could you present the evidence that some physicians and researchers give to support their claim that the pill is indeed an abortifacient?
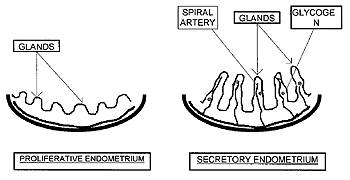
Before presenting the evidence, we should note what the normal anatomy and histology (ie, the study of the body's tissues on a microscopic level) of the inner lining of the uterus, (ie, the endometrium) looks like (see diagram B).
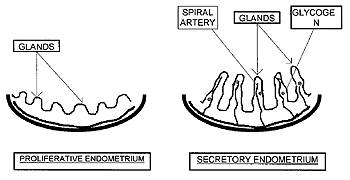
The endometrium slowly gets built up before ovulation (the proliferative phase) and then reaches its peak in the secretory phase (shortly after ovulation{and conception if it has occurred}). The endometrium is "ready for the newly conceived child to implant" when it reaches its peak in the secretory phase a few days after ovulation. We note that the blood flow and thus the oxygen and nutrients to the glandular cells of the endometrium increases through the cycle as the spiral arteries enlarge during the secretory phase. The size of the endometrial glands also enlarge in the secretory phase. The glands contain important nutritional building blocks for the unborn child who is about to implant, including glycogen (a type of sugar), mucopolysaccharides (ie, they supply certain building blocks for a cell's growth) and lipids (fats) 5.
3) What does the phrase "ready for implantation" mean?
The author of a histology text designed for medical students notes: "Thus, the various changes that take place in the endometrium during the second half of the menstrual cycle may be regarded as preparing the uterine lining for the nourishment and reception of the fertilized ovum (blastocyst)" 6. It would appear that God perfectly designed a woman's body and the lining of her uterus to be "optimal for implantation" a few days after ovulation and conception have occurred.
4) Does the OCP cause changes in the lining of the uterus that could be detrimental to the newly conceived child's ability to implant himself or herself?
It would appear so. Since we know that the oral contraceptive pill allows ovulation and conception to occur at times, if the pill causes unfavorable changes in the endometrium, it would make it difficult for the unborn child to implant, and would support the conclusion that it is an abortifacient.
5) What are some of those changes?
The first change that the OCP makes is to markedly decrease the thickness of a woman's endometrial lining. Women who take the pill know this because they can tell you that the volume of menstrual contents lost in their monthly cycles significantly decreases once they start taking the pill. Obviously if a woman is losing less menstrual contents each month, the layer of endometrium that is being shed must be thinner and less well developed.
6) Is there a technical or quantitative way to measure how much thinner a woman's endometrium becomes when she uses OCPs?
Yes, in 1991 researchers in the US performed MRI scans (Magnetic Resonance Imaging) on the uteri of women, some of whom were taking OCPs and some of whom were not 7. The OCP users had endometrial linings that were almost two millimeters thinner than that of the nonusers. Although this may sound like a small difference, it represented a 57% reduction in the thickness of the endometrial lining in women who used OCPs in this study.
7) But is there really any evidence that a thinner endometrium makes it more difficult for implantation to occur?
Yes. A number of different research papers have studied this issue and it has been widely described in the medical literature concerning in-vitro fertilization where it has been noted that the newly conceived child is much less likely to implant on a thinner uterine lining than a thicker one. Originally an older smaller study (Fleisher et al 8, 1985) did not find that the thickness of the endometrium played an important role in in-vitro implantation rates, however, other studies have noted a trend (Rabinowitz et al 9(1986); Ueno et al 10{1991}) or a statistically significant effect (Glissant et al 11, 1985) of the decreasing thickness of the endometrium in relationship to a decreased likelihood of implantation. Larger and more recent studies (Abdalla et al 12(1994); Dickey et al 13(1993); Gonen et al 14(1989); Schwartz et al 15(1997); Shoham et al 16{1991}) have reaffirmed this important connection. Most studies have noted that a decrease of even one millimeter in thickness yields a substantial decrease in the rate of implantation. In two studies, when the endometrial lining became too thin, no implantations occurred (Abdalla 12; Dickey 13).
8) What happens to the actual endometrial lining in women who take OCPs when one looks at it under a microscope?
As we noted in diagram B, the uterine lining is at an "optimal state for implantation" when the glands and uterine arteries are at their maximal size. This makes intuitive sense since at this point the blood supply and glycogen and lipid levels that the tiny unborn child needs to survive are at their maximal state. But what happens to the endometrium in women who take OCPs? It has already been noted that it becomes significantly thinner but what does it look like on the microscopic level?
Researchers who study the histology of the endometrium find that the OCP causes a number of effects. First, the spiral arteries regress significantly to the point where they are much smaller or even become difficult to find when one looks under a microscope 17-20. This of course is important, since an adequate blood supply is critical to the existence of the implanting unborn child. A loss of blood flow means a drastic curtailment in the food and oxygen supply that the child needs to survive. The blood flow to the endometrium is so important that in 1996 one researcher wrote directly about it as concerns its relationship to an unborn child's likelihood of implantation 21. She first noted that the blood flow through the spiral arteries peaks at day 16 to 18 of the menstrual cycle and then noted that: "It seems that endometrial perfusion presents more accurate noninvasive assay of uterine receptivity than uterine artery perfusion alone. Therefore, blood flow velocity waveform changes of spiral arteries may be used to predict implantation success rate to reveal unexplained infertility problems and to select patients for correction of endometrial perfusion abnormalities..." 21 (emphasis added)
9) Are there any other changes on the microscopic level in addition to the reduced blood supply from the spiral arteries?
Yes, the second prominent effect is that the endometrial glands become much smaller and the "mitotic rate" (rate of cell division) of the cells of the glands decreases 17-20. Obviously if the glands which supply the glycogen (sugar), mucopolysaccharides or lipids (fats) are compromised, the unborn child who needs those nutrients will have a more difficult time implanting and/or surviving.
10) Many of the studies that examined the endometrial lining are older and were performed when OCPs contained a much higher level of estrogen content (100 micrograms or more). Would the same effect be occurring with more recent OCPs?
Yes. First it should be mentioned that if you ask a woman who is taking lower dose OCPs about the amount of monthly menstrual contents that she loses, she will note that she loses significantly less after she started taking the OCP. Obviously if she is losing less menstrual contents then she is shedding less each month because the lining of the uterus has become thinner. But what about at the histologic level? Even studies which looked at OCPs which contain 50 micrograms of estrogen (a medium dose) and 0.5 mg of a progestin (eg, norgestrel) found that the spiral arteries and the endometrial glands "shrivel up." 18, 19
11) Is there any other new evidence that support the argument that OCPs act by causing an early abortion?
Yes. In 1996 a researcher names Stephen Somkuti published an article concerning the endometrium and a group of molecules called "integrins." 22 Integrins are a group of adhesion molecules that have been implicated as playing an important role in the area of fertilization and implantation. There are different types of integrins and it is believed that the endometrium is most receptive to implantation when it expresses certain types of integrins. Oral contraceptive pills change the type of integrins that the endometrial lining produces theoretically making it more difficult for the unborn child to implant. In the words of Dr. Somkuti: "These alterations in epithelial and stromal integrin expression suggest that impaired uterine receptivity is one mechanism whereby OCs exert their contraceptive action." 22
 12) Has anyone proven that the OCP causes early abortions?
12) Has anyone proven that the OCP causes early abortions?
In order to prove if and how often women are having abortions while taking OCPs one needs to be able to measure how often women become pregnant while taking them. But early pregnancy tests are currently not accurate enough to confirm pregnancy within the first week (although some researchers have been able to detect the hormonal changes in pregnancy as early as four days after conception 4, 4A). Until a very early pregnancy test is developed or until researchers physically measure how many abortions are occurring in women who take OCPs, one cannot state with absolute certainty if and how often OCPs cause early abortion. The most accurate description of the current evidence is as follows:
All of the evidence on a microscopic, a macroscopic and an immunological level strongly support the argument that the OCP causes an early abortion at times. Until further studies are done, we should take heed and act upon the current data.
13) Recently a group of physicians, many of whom are experienced obstetricians, wrote a booklet entitled: Hormonal Contraceptives: Are they Abortifacients?. In it they write that: "The 'hormonal contraception is abortifacient theory is not established scientific fact. It is speculation." Could you comment on why a group of physicians would hold this view and on the nature of their arguments?
An overview and rebuttal to the arguments cited in the booklet entitled "Hormonal Contraceptives: Are they Abortifacients?" is found in the appendix directly after the footnotes. This author believes that some of their own arguments can be shown to actually support the argument that the pill is an abortifacient.
Footnotes:
1) Faust JM. Image change for condoms. ABC News Report. [Internet E-mail]. 6/8/97.
2) Kahlenborn C. How do the pill and other contraceptives work? Life Advocate. July 1997; 20-25.
3) Smith, Janet. Contraception, why not? cOne More Soul. Dayton, OH (1-513-279-5433)
3A) Elstein M et al. Studies on low0dose oral contraceptives: cervical and plasma hormone changes in relation to circulationg d-norgestrel and 17alpha-ethyniyl estradiol concentrations. Fertility and Sterility. 27; 1976: 892-899.
3B) Wolf DP et al. Human cervical mucus v. oral contraceptives and mucus rheologic properties. Fertility and sterility. 32; 1979: 166-169.
3C) Chang MC, Hunt DM. Effects of various progestins and estrogen on the gamete transport and fertilization in the rabbit. Fertility and Sterility. 1970; 21: 683-686.
3D) Potter LA. How effective are contraceptives? The determination and measurement of pregnancy rates. Obstet Gynecol. 1996; 88: 13S-23S.
4) Witt B, Wolf G, et al. Relaxin, CA-125, progesterone, estradiol, Schwnagerschaft protein, and human chorionic gonadotropin as predictors of outcome in threatened and nonthreatened pregnancies. Fertility and Sterility. 1990; 53: 1029-1036.
5) Norman RJ et al. Inhibin and relaxin concentration in early singleton, multiple, and failing pregnancy: relationship to gonadotropin and steroid profiles. Fertility and Sterility. 1993; 59: 130-137.
6) Snell, Richard. Clinical and Functional Histology for the Medical Student. Little, Brown & Co. Boston; c 1984, 586-591.
7) Ibid.
8) Brown HK et al. Uterine Junctional Zone: Correlation between Histologic Findings and MR Imaging. Radiology. 1991; 1798: 409-413.
9) Fleischer AC et al, Sonography of the endometrium during conception and nonception cycles of in vitro fertilization and embryo transfer. Fertility and Sterility. 1986; 46: 442-447.
10) Rabinowitz R et al. The value of ultrasonographic endometrial measurement in the preciction of pregnancy following in vitro fertilization. Fertility and Sterility. 1986; 45: 824-826.
11) Ueno J et al. Ultrasonographic appearance of the endometrium in natural and stimulated in-vitro fertilization cycles and its correlation with outcome. Human Reproduction. 1991; 6: 901-904.
12) Glissant A et al. Ultrasound study of the endometrium during in vitro fertilization cycles. Fertility and Sterility. 1985. 44: 786-789.
13) Abdalla HI et al. Endometrial thickness: a predictor of implantation in ovum recepients? Human Reporduction. 1994; 9: 363-365.
14) Dickey RP et al. Relationship of endometrialthickness and pattern to fecundity in ovulation induction cycles: effect of clomiphene citrate alon and with human menopausal gonadotropin. Fertility and Sterility. 1993. 59: 756-760.
14) Gonen Y et al. Endometrial thickness and growth during ovarian stimulation: a possible predictor of implantation in in-vitro fertilization. Fertility and Sterility. 1989; 52: 446-450.
15) Schwartz LB et al. The embryo versus endometrium controversy revisited as it relates to predicting pregnancy outcome in in-vitro fertilization-embryo transfer cycles. Human Reproduction. 1997; 12: 45-50.
16) Shoham Z et al. Is it possible to run a succesful ovulation induction program based solely on ultrasound monitoring: The importance of endometrial measurements. Fertility and Sterility. 1991; 56: 836-841.
17) Hilliard George D, Norris HJ, Pathologic effects of oral contraceptives, Recent Results in Cancer Research. 1979. 66;49-71.
18) Ober WB. The effects of oral and intrauterine administration of contraceptives on the uterus. Human Pathology. 1977; 8: 513-527.
19) Ober WB. Synthetic progestagen-oestrogen preparations and endometrial morphology. J. Clin Path. 1966; 19: 138.
20) Roland M et al. Sequential endometrial alterations during one cycle of treatment with synthetic progestagen-estrogen compounds. 1966. 17: 339.
21) Kupesic S. The first three weeks assessed by transaginal color doppler. J. Perinat. Med. 1996; 24:301-317.
22) Somkuti SG et al. The effect of oral contraceptive pills on markers of endometrial receptivity. Fertility and Sterility. 1996. 65; 484-488.
23) DeCook JL, McIlhaney J et al. Hormonal Contraceptives: Are they Abortifacients: 1998; Frontlines publishing. Sparta, MI. For contact information call 1-616-887-6256. Email: order@frontlines.org
Appendix:
Response to the arguments put forth in the brochure entitled: Hormonal Contraceptives: Are they Abortifacients?
Introduction: In January, 1998, a group of twenty-two physicians (almost all were obstetricians) wrote a collaborative report regarding the question of the abortifacient nature of the pill A. Their four main arguments (found on page 7 in their booklet) and a corresponding rebuttal to each are presented:
1: They write: "We know of no existing scientific studies that validate the 'hormonal contraception is partly abortifacient' theory. 'On-pill' pregnancy rates roughly parallel 'on-pill' ovulation rates (about 3-5 percent on 35 mcg pill). Increased spontaneous abortion of on-pill pregnancies is not noted."
Response: The claim that "on-pill" pregnancy rates roughly parallel "on-pill" ovulation rates may at first appear to be a satisfying argument, but on closer examination, this argument actually bolsters the evidence that the pill is an abortifacient. Why?
If a woman is taking the pill she will experience an artificially regulated cycle that lasts 28 days and so she will have about 13 cycles per year (365 days divided by 28). Thus a group of 100 women would be expected to have a total of 1300 cycles per year. If 4% of these are breakthrough cycles, a group of 100 women would be expected to have 52 breakthrough cycles in one year (1300 x 4%). William's Obstetrics notes that on average, about one-third of a couple's cycles will result in fertility B, so on average we should expect about 17 pregnancies in this group (52 x 33%). But the PDR (Physician's Desk Reference) notes that a group of 100 women who are using the pill in a consistent manner will have about 3 pregnancies per year C. Even if we use Potter's updated statistics of 7 pregnancies per year (see source 3D above), we must ask: What happened to the remaining babies? That is, if we expect 17 pregnancies in such a group and note only seven, one must account for the remaining 10 babies, who theoretically failed to implant and were aborted at an early stage. Thus, the cited group of obstetricians' argument that breakthrough ovulation rates parallel pregnancy rates actually bolsters the evidence that the pill is an abortifacient.
One additional notation should be mentioned. This author has noted that researchers who study the pill's breakthrough ovulation rate appear to do so in women who have been taking the pill for less than one year D, E. It is quite possible that a woman's pituitary gland "resets itself" with time resulting in a far higher rate of breakthrough ovulation. This phenomenon was noted in a paper which studied the rate of breakthrough ovulation of Norplant. In the first year it was noted to be only 11%, but it increased dramatically after that year, so that a 7-year average yielded an annual breakthrough ovulation rate of 44% F. There is certainly an urgent need to perform studies that examine the rate of breakthrough ovulation in women who have been taking the pill for more than one year. If the rate of breakthrough ovulation increased after a year, the argument in favor of the pill's abortifacient nature would be exceedingly difficult to dispute.
2: They write: "There is regular successful implantation of the invasive blastocyst on surfaces a great deal more 'hostile' than 'hostile endometrium' (eg, fallopian tube lining). 'Hostile endometrium' is not a demonstrated clinical reality."
Response: This argument is specious. It has already been noted in the answers to questions 3-13 that the sum of the evidence__both recent and old__supports the argument that the pill changes the lining of the endometrium in an unfavorable fashion. The fact that the unborn child may attach him or herself to a structure such as the fallopian tube lining has little to do with the noted arguments. Although one can make the argument that a rare occurrence or an exception disproves a theory, one cannot deduce the converse, namely, that the exception proves the theory. That is, noting that some unborn children do implant in the fallopian tube, or for that matter in the peritoneal cavity, merely proves that it is possible for this event to occur. But it offers no evidence that justifies the claim that a favorable implantation cite is just as good as an unfavorable one.
3: They write: "The extremely rare reporting of ectopic pregnancies associated with hormonal contraception would indicate the rarity of actual conception by patients using these modalities."
Response: Once again the noted physicians apparently were unaware that their statement serves the purpose of supporting the pill's action as an abortifacient. It should be noted that both women who take the pill and those who do not, can become pregnant. The pregnancy can be an extrauterine pregnancy (EUP) {ie, usually an ectopic pregnancy} or intrauterine (IUP) {ie, the normal type of pregnancy}. One can measure the ratio of EUP to IUP in either group of women. What should happen to this ratio {ie, (EUP)/(IUP)} if one compares women who are not taking the pill to those who are?
The obstetricians would argue that since ectopic pregnancies (and thus EUPs) are much rarer when women take the pill, this ratio should decrease, since the numerator should become smaller. On the contrary, if the pill caused more early abortions (ie, less IUPs), one would expect the number of IUPs to decrease in comparison to the number of EUPs and thus the ratio should increase. What does the literature say?
The studies to date note that women who take the pill have an increased ratio of EUP to IUP. They note that women who take the pill are far more likely to experience more EUP's per IUP than women who do not take the pill, which supports the argument that the pill is an abortifacient. The odds ratio of the increased risk of EUP/IUP in women taking the pill compared to women who were not taking the pill were as follows:
1) WHO G found an odds ratio of 1.7 (1.1-2.5); 2) Mol et al H found an odds ratio of 1.8 (0.9-3.4); 3) Job-Spira et al I found an odds ratio of 4.3 (1.5-12.6); 4) Thorburn et al J found an odds ratio of 4.5 (2.1-9.6); and 5) Coste et al K found an odds ratio of 13.9 (1.8-108.3).
4: They write: "Many factors play a part in how a family plans and spaces their children. It is not the purpose of this paper to promote nor to oppose hormonal contraception."
Response: As a physician I know that it is common to use a medicine or a type of procedure because previous physicians have done so. It is simply impossible for each physician to "re-invent the wheel" when trying to decide if a particular drug or procedure is the optimal one. Unfortunately, once one becomes accustomed to particular ways of doing things, one tends to continue to do them in a particular fashion because "they have always been done that way," and "new thoughts" on a "standard procedure" are not always appreciated.
How do these statements pertain to the noted arguments? It has been noted that almost every physician who signed or helped write the booklet Hormonal Contraceptives: Are they Abortifacients? was an obstetrician. It is common knowledge that virtually all obstetricians prescribe the pill to their patients for the purpose of contraception, in addition to other uses. Therefore, I assume (and would immediately issue a retraction if I were proven wrong) that every obstetrician who signed or helped write the paper, either did or currently continues to use oral contraceptive pills as a means of contraception for his or her patients.
The problem here is that obstetricians who are self-proclaimed as being pro-life would have difficulty being unbiased towards the argument that the pill causes early abortions, since each of these physicians most likely has written thousands of prescriptions in his or her medical career. The admission of the pill as abortifacient amounts to an admission that hundreds of tiny unborn children have been aborted by the physicians who prescribed the pill. Would it not be difficult to expect a pro-life obstetrician to fairly evaluate the pill as an abortifacient when one considers these circumstances?
In conclusion, the arguments presented by the twenty-two physicians in the booklet entitled Hormonal Contraceptives: Are they Abortifacients? are lacking in substance and often serve to bolster the evidence that the oral contraceptive pill causes early abortions to occur.
Footnotes:
A) DeCook JL, McIlhaney J et al. Hormonal Contraceptives: Are they Abortifacients: 1998; Frontlines publishing. Sparta MI. For contact information call 1-616-887-6256. Email: order@frontlines.org
B) Cunningham et al. William Obstetrics, 20th Edition. Appleton and Lange. c 1997. Stanford, CT. p 580-1.
C) Physician's Desk Reference: 1997 {The noted information can be found when looking up any oral contraceptive. Failure rate for "typical use" is noted to be 3 percent.}
D) Editor : Chmaberlain G. Contemporary Obstetrics and Gynecology : Van der Vange N. Ovarian activity during low dose oral contraceptives. London. Butterworths, 1988.
E) Killick S et al. Ovarian folicular development in oral contraceptive cycles. Fertility and Sterility. 1987. 48; 409-413.
F) Croxatto HB, Diaz S, et al. Plasma progesterone levels during long term treatment with levonorgestrel silastic implants. Acta Endocrinologica; 1982; 101: 307-311.
G) The WHO Task Force on intrauterine devices for fertility regulation. A multinational case-control study of ectopic pregnancy. Clin Reprod Fertil 1985;3:131-143.
H) Mol BWJ, Ankum WM, Bossuyt PMM, and Van der Veen F. Contraception and the risk of ectopic pregnancy: a meta analysis. Contraception 1995;52:337-341.
I) Job Spira N, Fernandez H, Coste J, Papiernik E, Spira A. Risk of Chlamydia PID and oral contraceptives. J Am Med Assoc 1990;264:2072-4.
J) Thorburn J, Berntsson C, Philipson M, Lindbolm B. Background factors of ectopic pregnancy. I. Frequency distribution in a case-control study. Eur J Obstet Gynecol Reprod Biol 1986;23:321-331.
K) Coste J, Job-Spira N, Fernandez H, Papiernik E, Spira A. Risk factors for ectopic pregnancy: a case-control study in France, with special focus on infectious factors. Am J Epidemiol 1991;133:839-49.
This article will soon be available in brochure form. To obtain copies, contact One More SOul at (1-937-279-5433) [omsoul@juno.com].
OTHER
FEATURE
ARTICLES
The Oral Contraceptive Pill: Can a Christian afford to take it?
Sanger’s “plan for peace” has resulted in
never-ending culture war.

|
|